American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
CPT Primer for Psychiatrists
What is CPT?
Current Procedural Terminology (CPT) was first published by the American Medical
Association (AMA) in 1966. The CPT coding system was created to provide a uniform
language for describing medical and surgical procedures and diagnostic services that
would facilitate more effective communication between clinicians, third-party payers, and
patients. The 2013 CPT Manual is the most recent revision of the 4
th
edition of the book.
The AMA’s CPT Editorial Panel has the sole authority to revise, update, or modify CPT.
The panel has seventeen members, eleven nominated by the AMA, and one each from
the Blue Cross and Blue Shield Association, the Health Insurance Association of
American, the Centers for Medicare and Medicaid Services (formerly HCFA), the
American Hospital Association, and the Health Care Professionals Advisory Committee,
and one representative from the AMA/Specialty Society RVS Update Committee. In
1990, Tracy Gordy, M.D., became the first psychiatrist to be appointed to the panel. He
retired as chair of the panel in November 2007.
The CPT Editorial Panel is supported by the CPT Advisory Committee, which has
representatives from over 90 specialty societies. The committee’s main role is to advise
the editorial panel on procedural coding and nomenclature that is relevant to each
committee member’s specialty. The committee also serves as a conduit through which
revision to CPT can be proposed by specialty societies, or by individual members of
those specialty societies.
The AMA’s CPT coding system is now used almost universally throughout the United
States. The Transaction Rule of the Health Insurance Portability and Accountability Act
(HIPAA), which went into effect on October 16, 2002, requires the use of CPT codes by
all who are covered by HIPAA. The CPT codes comprise Level I of the HCPCS (Health
Care Financing Administration Common Procedure Coding System) codes used by
Medicare and Medicaid. Every healthcare provider who is paid by insurance companies,
or whose patients are reimbursed by insurance companies, should have a working
knowledge of the CPT system.
How Is the CPT Manual Organized?
The CPT manual is organized to be as user friendly as possible. The following is a quick
survey of its contents.
Introduction
The short introduction contains valuable information for the clinician on how to use the
manual, including:
A description and explanation of the format of the terminology (This section
describes how some routine procedural terms are not repeated for subsequent
related procedures to conserve entry space.);
A description of how to request updates of CPT (It is vital that physicians keep the
AMA aware of changes in practice that require coding changes.);
A discussion of the specific guidelines that precede each of the manual’s six
sections (E/M and the five clinical sections);

American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
A discussion of ―add-on codes‖ for additional or supplemental procedures;
An explanation of code modifiers and how they are to be used;
A brief discussion of how place of service relates to CPT;
A discussion of the inclusion of codes for unlisted procedures or services in each
section;
A note that some CPT codes require interpretation and reporting if they are to be
used;
A note that special reports may be required to determine the medical appro-
priateness of rare or very new services;
A discussion of how to identify code changes from year to year;
A reference to the expanded alphabetical index now included in the Manual;
A note on how to obtain electronic versions of CPT; and finally
How references to AMA resources on the CPT codes are noted in the Manual.
Illustrated Anatomical and Procedural Review
This section provides a review of the basics of anatomy and medical vocabulary that are
necessary for accurate coding. Lists of prefixes, suffixes, and roots are given, followed by
22 anatomical illustrations. There is also an index of all the procedural illustrations that
appear throughout the manual, listed by their corresponding codes.
Molecular Pathology
This is a new section in 2013.
Evaluation and Management Codes
Although the rest of the CPT manual is organized according to the numerical order of the
codes, the evaluation and management (E/M) codes, 99xxx, are provided in the first code
section because they are used by physicians in all specialties to report a considerable
number of their services. The E/M codes are preceded by tables that indicate the
required components for the various E/M codes and fairly extensive guidelines that define
the terms used in the code descriptors and provide instructions for selecting the correct
level of E/M service.
Major Clinical Sections
Next come the major clinical sections: Anesthesia, Surgery, Radiology, Pathology and
Laboratory, and Medicine. Each of these sections is preceded by guidelines. The
psychiatry codes, 908xx, are found in the Medicine section. The codes in the Psychiatry
subsection cover most of the services mental health professionals provide to patients in
both inpatient and outpatient settings.
Category II and III Codes
The Medicine section is followed by a listing of the supplemental Category II and
Category III codes. These codes are generally optional codes used to facilitate data
collection and are never used as substitutes for the standard Category I CPT codes.
Category II codes are used for performance measurement. According to the CPT
Manual, Category II codes are ―intended to facilitate data collection about the quality of
care rendered by coding certain services and test results that support nationally
established performance measures and that have an evidence base as contributing to

American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
quality patient care.‖ These codes will be used more and more as Medicare attempts to
shift from volume-based payment to quality-based payment.
Category III codes are temporary codes that are used to allow data tracking for emerging
services and procedures.
Appendixes and Index
The last section of the manual includes appendixes and an extensive alphabetical index.
There are 13 appendixes:
1. Appendix A: Modifiers—modifiers are two-digit suffixes that are added to CPT codes
to indicate that the service or procedure has been provided under unusual
circumstances (e.g., –21, which indicates a prolonged E/M service) (See Appendix B
of this book for a list of modifiers.)
2. Appendix B: Summary of Additions, Deletions, and Revisions (of codes in the current
manual)
3. Appendix C: Clinical Examples—provides clinical examples to clarify the use of E/M
codes in various situations
4. Appendix D: Summary of CPT Add-On Codes—codes used to denote procedures
commonly carried out in addition to a primary procedure
5. Appendix E: Summary of CPT Codes Exempt From Modifier –51 (multiple
procedures)
6. Appendix F: Summary of CPT Codes Exempt From Modifier –63 (which denotes a
procedure perfomed on infants)
7. Appendix G: Summary of CPT Codes That Include Moderate (Conscious) Sedation
8. Appendix H: Alphabetic Index of Performance Measures by Clinical Condition or
Topic (a listing of the diseases, clinical conditions, and topics with which the Category
II codes are associated.)
9. Appendix I: Genetic Testing Code Modifiers (used
―to
provide diagnostic granularity of
service to enable providers to submit complete and precise genetic testing information
wihout altering test descriptors.‖)
10. Appendix J: Electrodiagnostic Medicine Listing of Sensory, Motor, and Mixed Nerves
11. Appendix K: Products pending FDA Approval (vaccine products that have been
assigned a Category I codes in anticipation of their approval)
12. Appendix L: Vascular Families
13. Appendix M: Crosswalk to Deleted CPT Codes (indicating which current codes are to
be used in place of the deleted ones)
The index is preceded by instructions explaining that there are four primary classes of
index entries:
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
1. Procedure or Service
2. Organ or Other Anatomic Site
3. Condition
4. Synonyms, Eponyms, and Abbreviations
The instructions also explain the index’s use of modifying terms, code ranges, and space-
saving conventions.
Psychiatry Codes
The codes most frequently used by psychiatrists can be found in the Psychiatry subsection of
the Medicine section of the CPT Manual (codes 90785-90899). For 2013 and beyond there
have been major changes to the Psychiatry codes. A distinction has been made between an
initial evaluation with medical services done by a physician (90792) and an initial evaluation
done by a non-physician (90791). The psychotherapy codes have been simplified: There are
now three timed codes to be used in all settings (90832- 30 minutes; 90834-45 minutes;
90837- 60 minutes) and accompanying add-on codes for psychotherapy (indicated in CPT by
the + symbol in the CPT Manual) that are to be used by psychiatrists when the psychotherapy
is provided in the same encounter as medical evaluation and management (90833 -30
minutes, 90836 - 45 minutes, 90838 – 60 minutes). In lieu of the codes for interactive
psychotherapy, there is now an add-on code for interactive complexity (90785) that may be
used with any code in the Psychiatry section for which it is appropriate. Another change is
that a new code has been added for psychotherapy for a patient in crisis (90839). When a
crisis encounter goes beyond 60 minutes there is an add-on code for each additional 30
minutes (90840). Code 90862 has been eliminated, and psychiatrists will now use the
appropriate evaluation and management (E/M) code when they do pharmacologic
management for a patient. (A new code, add-on code 90863, has been created for medication
management when done with psychotherapy by the psychologists in New Mexico and
Louisiana who are permitted to prescribe, but this code is not to be used by psychiatrists or
other medical mental health providers). All of these changes are discussed in detail below.
Interactive Complexity Add-On
90785 Interactive Complexity -- This add-on code may be used with any of the codes in
the Psychiatry section when the encounter is made more complex by the need to involve
others than the patient. It will most frequently be used in the treatment of children. When
this add-on is used, documentation must explain what exactly the interactive complexity
was (i.e., the need for play equipment with a younger child; the need to manage parents’
anxiety; the involvement of parents with discordant points of view).
What is an add-on code? An add-on code is a code that can only be
used in conjunction with another code and is indicated by the plus
symbol (+) in the CPT manual. While basic CPT codes are valued to
account for pre- and post-time, add-on codes are only valued based
on intra-service time since the pre- and post-time is accounted for in
the basic code. In the new Psychiatry codes there are three different
types of add-on codes: 1.) Timed add-on codes to be used to indicate
psychotherapy when it is done with along with medical evaluation and
management; 2.) A code to be used when psychotherapy is done that
involves interactive complexity (e.g., psychotherapy provided to
children or geriatric patients who have difficulty communicating without
assistance); and 3.) A code to be used with the crisis therapy code
for each 30 minutes beyond the first hour.
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
Psychiatric Diagnostic Evaluation Codes
90791Psychiatric Diagnostic Evaluation – This code is used for an initial diagnostic
interview exam that does not include any medical services. In all likelihood this code will not
be used by psychiatrists. It includes a chief complaint, history of present illness, family and
psychosocial history, and complete mental status examination. In the past most insurers
would reimburse for one 90791 (then a 90801) per episode of illness. The guidelines now
allow for billing this on subsequent days when there is medical necessity for an extended
evaluation (i.e., when an evaluation of a child that requires that both the child and the
parents be seen together and independently). Medicare will pay for only one 90791 per
year for institutionalized patients unless medical necessity can be established for others.
90792Psychiatric Diagnostic Evaluation with Medical Services– This code is used for
an initial diagnostic interview exam for an adult or adolescent patient that includes medical
services. It includes a chief complaint, history of present illness, review of pertinent systems,
family and psychosocial history, and complete mental status examination, as well as any
medical work such as the ordering and medical interpretation of laboratory or other diagnostic
studies or the prescribing of medications. In the past most insurers would reimburse for one
90792 (then a 90801) per episode of illness. The guidelines now allow for billing this on
subsequent days when there is medical necessity for an extended evaluation (i.e., when an
evaluation of a child that requires that both the child and the parents be seen together and
independently).
Medicare will pay for only one 90792 per year for institutionalized patients unless medical
necessity can be established for others. Medicare permits the use of this code or the
appropriate level of the E/M codes (see below) to denote the initial evaluation or first-day
services for hospitalized patients. Medicare also allows for the use of 90792 if there has been
an absence of service for a three-year period.
For 2013, it is important to note that both codes 90791 and 90802 are not subject to the
outpatient mental health services limitation under Medicare that will be eliminated in 2014.
They have always been reimbursed at 80% like all other medical codes.
Psychiatric Therapeutic Procedure Codes
There are now three basic timed individual psychotherapy codes, which are to be used in all
settings and add-on codes to be used when psychotherapy is done along with medical
evaluation and management and/or when psychotherapy is provided for a patient when there
is interactive complexity. Note that the descriptors for the psychotherapy codes now list the
time as the time spent ―with patient and/or family member,‖ rather than ―face- to-face with the
patient‖ as for the previous psychotherapy codes.
+90785, the system complexity add-on code, may be used with these codes
90785, the system complexity add-on code, may be used with all of these codes
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
Another difference is the way time is now defined by CPT. The CPT manual has
standards in place that are to be used when selecting codes that have a time attached to
them, except when rules are stipulated within the codes themselves. The bullets below
will provide you with the basics for coding for psychiatric services.
Time is only the time spent face-to-face with the patient and/or family member.
When codes have sequential typical times attached to them, as with the basic
psychotherapy codes, the code that is closest to the typical time should be
selected.
A unit of time is attained when the mid-point is passed. (For example, if you see a
patient for more than 15 minutes you may code using 90832, the 30-minute code;
and if you see a patient for 35 minutes, you would also use 90832. However, if
you see the patient for 38 to 52 minutes, you would use 90834, the 45-minute
code; and for 53 minutes or more you would use 90837, the 60-minute code).
90832 Individual Psychotherapy, 30 minutes with patient and/or family member
90833 Individual Psychotherapy, 30 minutes with patient and/or family member
when performed with an evaluation and management service (list separately in
addition to the code for the primary procedure.)
90834 Individual Psychotherapy, 45 minutes with patient and/or family member
90836 Individual Psychotherapy, 45 minutes with patient and/or family member
when performed with an evaluation and management service (list separately in
addition to the code for the primary procedure.)
90837 Individual Psychotherapy, 60 minutes with patient and/or family member
90838 Individual Psychotherapy, 60 minutes with patient and/or family member
when performed with an evaluation and management service (list separately in
addition to the code for the primary procedure.)
Other Psychotherapy Codes
90845Psychoanalysis – Psychoanalysis is performed by therapists who are trained
and credentialed to practice it. Psychoanalysis is reported on a per-session basis and is
reimbursed by most insurance programs. The issue of medical necessity has resulted in
challenges to reimbursement for psychoanalysis by managed care companies. Note that
90845 is not a time-based code.
90846Family Psychotherapy (Without the Patient Present) – This code is used
when the psychiatrist provides therapy for the family of a patient without the patient being
present. Under Medicare rules, 90846 is only covered if the therapy is clearly directed
toward the treatment of the patient, rather than to treating family members who may have
issues because of the patient’s illness. While most insurance companies will reimburse
for this code, problems may occur because the service is not face-to-face with the
patient.
90847Family Psychotherapy (Conjoint Psychotherapy) (With Patient Present) –
This code is used when the therapy includes the patient and family members. It is
90785, the system complexity add-on code, may be used with all of these codes
-30-
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
covered by most insurance plans, and is challenged less often than 90846 because the
patient is present. It should also be used for couples therapy.
90849Multiple-Family Group Psychotherapy – This code is used when the
psychiatrist provides psychotherapy to a group of adult or adolescent patients and their
family members. The usual treatment strategy is to modify family behavior and attitudes.
The service is covered by most insurance plans.
90853Group Psychotherapy (Other Than of a Multiple-Family Group) – This code
relies on the use of interactions of group members to examine the pathology of each
individual within the group. In addition, the dynamics of the entire group are noted and
used to modify behaviors and attitudes of the patient members. The size of the group
may vary depending on the therapeutic goals of the group and/or the type of therapeutic
interactions used by the therapist. The code is used to report per-session services for
each group member. Most insurance plans cover this procedure.
Codes for Other Psychiatric Services or Procedures
90865Narcosynthesis for Psychiatric Diagnostic and Therapeutic Purposes (e.g.
sodium amobarbital (Amytal) interview) – This procedure involves the administration,
usually through slow intravenous infusion, of a barbiturate or a benzodiazepine in order to
suppress inhibitions, allowing the patient to reveal and discuss material that cannot be
verbalized without the disinhibiting effect of the medication. This code is reimbursed by
most insurers.
90867Therapeutic Repetitive Transcranial Magnetic Stimulation (TMS) initial
treatment, including cortical mapping, motor threshold determination, delivery and
management
90868Subsequent TMS Delivery and Management, per session
90869Subsequent TMS Motor Threshold Re-Determination with Delivery and
Management
90870Electroconvulsive Therapy (Includes Necessary Monitoring); Single seizure –
This code is for electroconvulsive therapy (ECT), which involves the application of electric
current to the patient’s brain for the purposes of producing a seizure or series of seizures
to alleviate mental symptoms. ECT is used primarily for the treatment of depression that
does not respond to medication. The code includes the time the physician takes to
monitor the patient during the convulsive phase and during the recovery phase. When
the psychiatrist also administers the anesthesia for ECT, the anesthesia service should
be reported separately, using an anesthesia code. ECT is covered by most insurance
plans.
90875Individual Psychophysiological Therapy Incorporating Biofeedback
Training by any Modality (face-to-face with the patient), With Psychotherapy (e.g.,
insight-oriented, behavior modifying, or supportive psychotherapy); approximately 20-30
minutes and,
90876approximately 45-50 minutes

-31-
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
These two procedures incorporate biofeedback and psychotherapy (insight oriented,
behavior modifying, or supportive) as combined modalities conducted face-to-face with
the patient. They are distinct from biofeedback codes 90901 and 90911, which do not
incorporate psychotherapy and do not require face-to-face time. Medicare will not
reimburse for either of these codes.
90880Hypnotherapy – Hypnosis is the procedure of inducing a passive state in which
the patient demonstrates increased amenability and responsiveness to suggestions and
commands, provided they do not conflict seriously with the patient’s conscious or
unconscious wishes. Hypnotherapy may be used for either diagnostic or treatment
purposes. This procedure is covered by most insurance plans.
90882Environmental Intervention for Medical Management Purposes on a
Psychiatric Patient’s Behalf With Agencies, Employers, or Institutions – The
activities covered by this code include physician visits to a work site to improve work
conditions for a particular patient, visits to community-based organizations on behalf of a
chronically mentally ill patient to discuss a change in living conditions, or accompaniment
of a patient with a phobia in order to help desensitize the patient to a stimulus. Other
activities include coordination of services with agencies, employers, or institutions. This
service is covered by some insurance plans, but because some of the activities are not
face-to-face, the clinician should check with carriers about their willingness to reimburse
for this code.
90885Psychiatric Evaluation of Hospital Records, Other Psychiatric Reports,
Psychometric and/or Projective Tests, and Other Accumulated Data for Medical
Diagnostic Purposes – Although this would seem to be a very useful code, because
reviewing data is not a face-to-face service with the patient, Medicare will not reimburse
for this code and some commercial carriers have followed suit. Medicare considers the
review of data to be part of the pre-/postwork associated with any face-to-face service.
90887Interpretation or Explanation of Results of Psychiatric, Other Medical
Examinations and Procedures, or Other Accumulated Data to Family or Other
Responsible Persons, or Advising Them How to Assist Patient – Medicare will not
reimburse for this service because it is not done face-to-face with the patient, and
clinicians should verify coverage by other insurers to ensure reimbursement. It is
appropriate to use an E/M code in the hospital where floor time is expressed in
coordination of care with the time documented.
90889Preparation of Report of Patient’s Psychiatric Status, History, Treatment, or
Progress (Other Than for Legal or Consultative Purposes) for Other Physicians,
Agencies, or Insurance Carriers – Psychiatrists are often called upon to prepare
reports about the patient for many participants in the healthcare system. This code would
be best used to denote this service. However, because this is not a service provided
face-to-face with a patient, Medicare will not reimburse for this code either, and clinicians
should verify coverage by other insurers.
90899Unlisted Psychiatric Service or Procedure – This code is used for services not
specifically defined under another code. It might also be used for procedures that require
some degree of explanation or justification. If the code is used under these
-32-
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
circumstances, a brief, jargon-free note explaining the use of the code to the insurance
carrier might be helpful in obtaining reimbursement. If it is used for a service that is not
provided face-to-face with a patient, the psychiatrist should check with the patient’s
insurer regarding reimbursement.
95970, 95974, 95975Neurostimulators, Analysis–Programming – These codes have
been approved for vagus nerve stimulation (VNS) therapy for treatment-resistant
depression. Clinicians performing VNS therapy should use the appropriate code from the
95970, 95974, and 95975 series of codes found in the neurology subsection of the CPT
manual. Medicare will not reimburse for these codes.
M0064Brief Office Visit for the Sole Purpose of Monitoring or Changing Drug
Prescriptions Used in the Treatment of Mental Psychoneurotic and Personality
Disorders – M0064 is not, in fact, a CPT code. It is a HCPCS Level II code (CPT codes
are HCPCS Level I), part of the HCPCS system used by Medicare and Medicaid. M0064
should only be used for the briefest medication check with stable patients.
Evaluation and Management Codes
With the elimination of code 90862 and the addition of the add-on codes for
psychotherapy when done with evaluation and management (E/M), psychiatrists will be
using far more E/M codes than they have in the past. Previously, many psychiatrists just
used the E/M codes for their inpatient and nursing facility encounters, but now they will
be used for outpatient care as well.
The evaluation and management codes were introduced in 1992 to cover a broad range
of services for patients, in both inpatient and outpatient settings. E/M code descriptors
provide explicit criteria for selecting codes, and the clinical vignettes given in Appendix C
of the CPT Manual provide examples of situations that fulfill these criteria.
Evaluation and management codes cover a family of general medical services provided in
various settings, i.e., office, hospital, nursing home, emergency department, etc. While
E/M codes are frequently used for hospital inpatient services, inpatient and outpatient
consultations, and nursing facility services; they are less frequently used in psychiatry for
office and other outpatient services, emergency department services, and domiciliary,
rest home services. It is extremely important to read the guidelines to the Evaluation
and Management section of the CPT Manual because they explain how to choose the
appropriate level of service when using E/M codes.
Level of Service
The level of service for an E/M code encompasses the skill, effort, time, responsibility,
and medical knowledge necessary to evaluate, diagnose, and treat medical conditions.
There are seven components that are used to define E/M levels of service:
history,
examination,
medical decision making,
counseling,
coordination of care,
nature of presenting problem, and
time.
-33-
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
The three key components used in selecting the level of service within each category or
subcategory of E/M service are:
the extent of the history
the extent of the examination
the complexity of medical decision making involved
The clinician’s ability to determine the appropriate level of service being provided to the
patient within each category or subcategory of evaluation and management services is
dependent on a thorough understanding of the Definition of Terms (found in the
Evaluation and Management Services Guidelines that precede the listing of the E/M
codes in the CPT Manual) and the Instructions for Selecting a Level of E/M Service (also
in the Guidelines). The brief synopsis that follows is not an adequate substitute for a
careful review of these sections of the CPT Manual.
There are three to five levels of service for each category or subcategory of E/M services.
Each level of service represents the total work (skill, time, effort, medical knowledge, risk)
expended by the clinician during an incident of service. For example, outpatient E/M
codes are divided by new patient and established patient, with five levels of service for
new patient care (99201-99205) and five for established patient care (99211-99215).
Each of the levels is based on the depth of history and examination and complexity of the
decision making involved, and the descriptors for the codes provide a typical time for the
code as well.
Consultations are divided into office or other outpatient consultations, initial inpatient
consultations. There are five levels of service for office consultations (99241-99245), and
initial inpatient consultations (99251-99255). Consultations are provided at the request of
another healthcare provider to whom a written report must be given. The CPT Editorial
Panel voted to delete the follow-up inpatient consultations and the confirmatory
consultations. The appropriate E/M service code (i.e., Established patient, office or other
outpatient service) should be used based on the setting and type of service. Clinicians
should become thoroughly familiar with the descriptors and codes within each family of
services as well as with the guidelines that spell out the methodology for selecting the
level of service provided. Medicare no longer pays for the consultation codes and some
commercial insurers have eliminated them as well.
History
There are four levels of history in the E/M codes: problem focused, expanded problem
focused, detailed, and comprehensive. The more detailed the history, the greater the
work effort.
Examination
The same four categories define the examination: problem focused, expanded problem
focused, detailed, and comprehensive. The more extensive the examination, the greater
the work effort. For psychiatry, a complete mental state examination (single system
examination) qualifies as a comprehensive examination.
Decision Making
There are four levels of medical decision making presented in the E/M codes: 1.
Straightforward; 2. Low complexity; 3. Moderate complexity; and 4. High complexity. The
more complex the medical decision making, the greater the work effort.
-34-
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
The complexity of the medical decision making depends on: the number of diagnoses or
management options; the amount and/or complexity of data to be reviewed; and the risk
of complications and/or morbidity or mortality.
For example, the lowest level of service for Office or Other Outpatient Consultations
(99241) requires:
a problem focused history;
a problem focused examination; and
straightforward medical decision making
Average time: 15 minutes
While the highest level of service for Office or Other Outpatient Consultations (99245)
requires:
a comprehensive history;
a comprehensive examination; and
medical decision making of high complexity
Average time: 80 minutes
The clinician selects 99241 or 99245 (or any of the levels in between, 99242, 99243,
99244) on the basis of the work performed (i.e., extent of history and examination,
complexity of medical decision making). The average times given for each code are
guidelines for the clinician and are not a requirement when using the key components
(history, examination, and medical decision making) in selecting the level of service.
Time and Level of Service
Time (as a component in selecting the level of service) has two definitions in the E/M
guidelines. The clinician must review these definitions (see CPT 2010, E/M Services
Guidelines) in order to fully understand the rationale for the two definitions.
For office and other outpatient visits and office consultations, intraservice time is defined
as the face-to-face time spent providing services to the patient and/or family members.
Time spent pre- and post-service (time that is not face-to-face) is not included in the
average times listed for office and outpatient consultation services. The work associated
with the pre- and post-encounter time has been calculated into the total work that forms
the basis for how each code is reimbursed, and, therefore, the average face-to-face times
listed with each E/M code are considered fair proxy for the total work effort.
For inpatient hospital care, hospital consultations, and nursing facility care intraservice
time is defined as unit floor time. Unit floor time includes all work the clinician performs
on behalf of the patient while present on the unit or at the bedside. This work includes
direct patient contact, review of chart, writing orders, reviewing test results, writing
progress notes, meeting with the treatment team, telephone calls, and meeting with the
family. Pre- and post-time work such as reviewing patient records in another part of the
hospital has been included in the calculation of total work as described above in the
definition of face-to-face time.
There is one final and important twist in using time in the selection of the level of service.
When counseling and/or coordination of care (see Physicians Current Procedural
Terminology 2013 , page 10) accounts for more than 50 percent of the patient and/or
family encounter unit/floor time, then time becomes the key factor in selecting level of

-35-
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
service. The clinician makes the selection by matching the time of the encounter (face-
to-face or unit/floor) to the average time listed for the appropriate E/M service. In this
instance there is no consideration of the extent of the history, the exam, the medical
decision making required, or the nature of the presenting problem; time is the sole
determinant.
Counseling is defined as a discussion with the patient and/or family concerning one or
more of the following: diagnostic results, prognosis, risks and benefits of treatment,
instructions for management, compliance issues, risk factor reduction, patient and family
education. Coordination of care entails discussions about the patient’s care with other
providers or agencies. These two services are considered contributory factors and
although important to E/M service, are not required to be provided at every encounter.
The following are examples of counseling and coordination of care. A clinician spends 35
minutes on the hospital floor (third hospital day for patient) and over 50 percent of that
time was spent in counseling and/or coordination of care. The correct code is 99233
(subsequent hospital care), average time 35 minutes. In this case, history, examination,
and medical decision making are no longer the factors that determine the selection of the
level of service. Instead, the clinician documents the extent of the
counseling/coordination of care in the daily progress note.
A patient returns to a psychiatrist’s office for a medication check. The encounter takes a
total of 25 minutes, during which time more than 12.5 minutes is spent explaining to the
patient about how a newly prescribed medication works, how to establish a routine so
that no doses will be missed, and the possible side-effects of the medication and what to
do if they occur. The appropriate E/M code would be 99214 (office or outpatient service
for an established patient), based on the 25-minute time rather than on a detailed history
and examination and moderately complex medical decision making that would be
required to use this code if counseling and coordination had not taken up more than 50
percent of the time.
Use of Modifiers
Modifiers are two-digit suffixes (e.g., –22, Unusual Procedure Services) that are added to
procedural codes to indicate the service or procedure has been provided under unusual
circumstances. The modifiers most likely to be used by psychiatrists are:
–22 Unusual Procedure Services
This modifier is used when the work associated with the service provided is greater
than that usually required for the listed code.
–25 Significant, Separately Identifiable Evaluation and Management Service by
the Same Physician on the Same Day of the Procedure or Other Service
This modifier is used to indicate that on the day a procedure or service identified by a
CPT code was performed, the patient’s condition required a significant, separately
identifiable E/M service above and beyond the other service provided or beyond the
usual pre- and postoperative care associated with the procedure performed.
–26 Professional Component
This modifier is used for procedures that are a combination of a physician component
and a technical component. When the physician component is reported separately,
this modifier is added to the usual procedure.

-36-
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
–52 Reduced Services
This modifier is used to report a service that is reduced in time.
The following is an example of how to use modifiers:
The therapy session requires extension from 50 minutes to 65 minutes because of the
emergence of important material just before the session was scheduled to end. The
session would be coded 90806-22 and a short explanatory note should be appended to
the insurance form, explaining the use of the code.
Documentation
Documentation is an extremely complex issue, an issue we can only touch on here. For
example, there may be special documentation requirements for Medicare found in the
local Medicare contractor’s Local Coverage Determination (LCD) policies; or when
psychiatrists use E/M codes for treating Medicare patients, the HCFA (CMS)
documentation guidelines should be used (but the clinician must decide whether to use
the 1995 or 1997 guidelines—see below); and commercial insurers may have their own
requirements.
Although accurate documentation of services and procedures is vital for good medicine,
documentation has become an increasingly troublesome practical issue for clinicians. It
is especially problematic for psychiatrists because of confidentiality issues and the
amount of clinical information produced during psychotherapy sessions. Also,
documentation for psychotherapy codes is one issue, while documentation for E/M codes
is another.
In 1995 the Health Care Financing Administration published documentation guidelines for
evaluation and management services. In 1997 revised E/M documentation guidelines
were issued. Currently, physicians can choose to base their documentation on either
the 1995 or 1997 Documentation Guidelines for Evaluation and Management Services.
Following either set will fulfill documentation requirements to the satisfaction of the
Medicare program, and should be acceptable to private insurers as well. Generally,
psychiatrists will want to use the 1997 guidelines, which allow for a single-system
psychiatric exam.
The Health Insurance Portability and Accountability Act (HIPAA), which was approved in
December 2000 and became effective in April 2001, has very specific requirements for
the privacy of patient records, and has very clear ramifications for the documentation of
psychotherapy. HIPAA distinguishes between psychotherapy notes (notes a therapist
may keep about the patient’s personal life as distinguished from the patient’s medical
history and treatment) and the medical record, and holds these personal notes to a
higher level of confidentiality. Since 2003, when all physicians were expected to be in
compliance with HIPAA, the standard of practice is that psychotherapy notes be kept so
that they can be easily separated from the rest of a patient record.
Reimbursement Issues
It is very important for the clinician to understand that just because a code exists for a
service in the CPT Manual, this does not guarantee that an insurance carrier or third-
party payer will reimburse for that code. For example, Medicare will not pay for code
90882, Environmental Intervention, nor will it pay for certain codes done on the same day
as others. You need to be aware of these exceptions. Clinicians may also find their
contracts with managed care organizations specify certain codes that are not

-37-
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
reimbursable, or that patients’ insurance policies specify certain services that are not
covered. It is essential to find out about any of these issues before treatment begins.
RBRVS and Medicare Reimbursement Policies
Because Medicare’s Resource-Based Relative Value Scale (RBRVS) system for the
payment of clinicians has become the basis of fee schedules, even for commercial
carriers, a discussion of coding issues associated with Medicare reimbursement is useful
even for those psychiatrists who do not treat Medicare beneficiaries.
Since 1992, the Medicare program has reimbursed physician services based on the
Resource-Based Relative Value Scale (RBRVS). RBRVS is a system that allows the
mathematical calculation of Relative Value Units (RVUs) for every CPT code. The cost of
providing each service described in CPT is divided into three components: physician
work, practice expense, and professional liability insurance. RVUs are assigned to each
component, then added together and multiplied by a conversion factor that is determined
annually by CMS and voted on by Congress. The resulting figure is the Medicare fee for
each service. Medicare fees vary slightly throughout the country due to adjustments for
geographical differences in resource costs. For instance, the fees in New York are
higher than those in Mississippi.
Medicare generally excludes from payment all non-face-to-face services such as
telephone calls, environmental interventions, record reviews, and case management,
although there may be some variation in local payment policies.
The way to avoid delay of payment or audits because of disputes over use of codes that
you’re not absolutely certain about is to prospectively negotiate with insurers about the
use of any codes that are not unquestionably standard.
Conclusions
Careful, correct coding is vital to the practicing psychiatrist. Take it seriously. Not only
will correct coding help achieve prompt and appropriate payment for treatment, it will also
provide protection from charges of fraud and abuse. Accurate documentation of the
services you have provided, and coded for, is the most certain means of protection
against allegations of abusive or fraudulent billing. Accurate documentation is also
extremely helpful in defending against malpractice allegations. You need to stay current
on coding issues.
Buy and read the AMA’s annually published CPT Manual
Stay in touch with your District Branch and the APA’s Office of Healthcare
Systems and Financing about coding and billing issues.
Psychiatrists who provide services under Medicare must educate themselves on
policies specific to Medicare. You must be sure to read any correspondence sent
to you by your Medicare contractor.
You should code and bill for all services rendered regardless of local or national payer
policies – the developing database may help change payment policies that negatively
affect reimbursement of mental health services.
It is important that you not try to game the reimbursement system by manipulating codes
inappropriately. Medicare/Medicaid fraud, and insurance fraud in general, is a serious
priority of the Justice Department.
-38-
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
Note: Although psychiatrists are likely to use only the codes within the Psychiatry and
E/M sections of the CPT Manual to cover the services they provide, the Manual clearly
states in its introduction: “Any procedure or service in any section of this book may
be used to designate the services rendered by any qualified physician.”
Recommended Reading
American Medical Association, Physicians Current Procedural Terminology
(published yearly, refer to most current)
APA’s Web Site, CPT Coding Service and Additional Resources
APA CPT Coding Service
Look for timely information on coding and documentation issues on the APA’s website
www.psychiatry.org in the Practice section and in the Psychiatric News Bulletin, which is
e-mailed to members weekly.
The APA is actively involved in making sure that members are correctly reimbursed for
the services they provide. Working closely with the Committee on RBRVS, Codes, and
Reimbursement, the APA’s Office of Healthcare Systems and Financing (OHSF) has
established a CPT Coding Service. Because CPT questions are very specific and often
very complex, a protocol has been established for queries to ensure that there will be no
misunderstanding.
APA members with CPT coding questions should:
Write an e-mail or memo with their name, APA member number, city, state, phone
number, fax number, and e-mail address.
State the question or describe the problem thoroughly, but succinctly—a short
paragraph is usually all that is necessary.
Include any relevant correspondence from Medicare carriers, insurance companies,
or third-party payers.
Cite any actions that have been taken relating to the problem, i.e., calls made, letters
written
E-mail (hsf@psych.org), fax (907-703-1089), or mail (Office of Healthcare Systems
and Financing, APA, 1000 Wilson Boulevard, # 1825, Arlington, VA, 22209) the
question to the attention of Rebecca Yowell.
All questions will be answered as quickly as possible.

-39-
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
Courses/Workshops
APA Annual Meeting Course and Workshop – A CPT coding CME course as well as a
CPT workshop are generally held each year at the APA Annual Meeting. Check the APA
Annual Meeting program for more information.
APA Medicare Advisory Network
The APA’s Office of Healthcare Systems and Financing maintains an online network of
psychiatrists who are involved in Medicare policy issues across the country. This network
allows the APA’s central office to monitor how Medicare is actually working from state to
state. It alerts psychiatrists across the United States to issues that are problematic and
keeps them apprised as to whether their state’s carrier is in compliance with Medicare
rules and regulations.
The network’s membership has historically been comprised of the psychiatry
representatives to each Medicare carrier’s Carrier Advisory Committee (CAC). Until very
recently Medicare carriers have administrated Part B of Medicare (Part A has been
administered by fiscal intermediaries), and the CACs have been mandated by law to
ensure that carriers have input from medical practitioners when they establish local
Medicare policy, specifically local coverage determinations, or LCDs; (formerly referred to
as LMRPs, or local medical review policies). The psychiatry representatives to the CACs
are chosen by the APA’s District Branches. Medicare has almost completed the
transition from carriers and fiscal intermediaries to Medicare Administrative Contractors,
which oversee both Parts A and B. Thus far it appears that the CACs will continue to
meet to advise these new entities just as they have Medicare carriers.
The Office of Healthcare Systems and Financing (OHSF) provides staffing for the
network and provides support so that members in all regions can work together when
there are issues that need to be addressed. Members of OHSF staff meet as necessary
with representatives from the Centers for Medicare and Medicaid Services and with
Medicare Medical Directors to solve problems communicated to them by members of the
network.
For information on your local representative to the APA Medicare network representative,
go to the APA web site at www.psychiatry.org. You can locate the list in the
Medicare/Medicaid section under Psychiatric Practice. Medicare questions can also be
directed to the attention of Ellen Jaffe in the Office of Healthcare Systems and Financing
(HSF) by calling 800-343-4671 or writing her via the HSF e-mail address, hsf@psych.org.

-40-
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
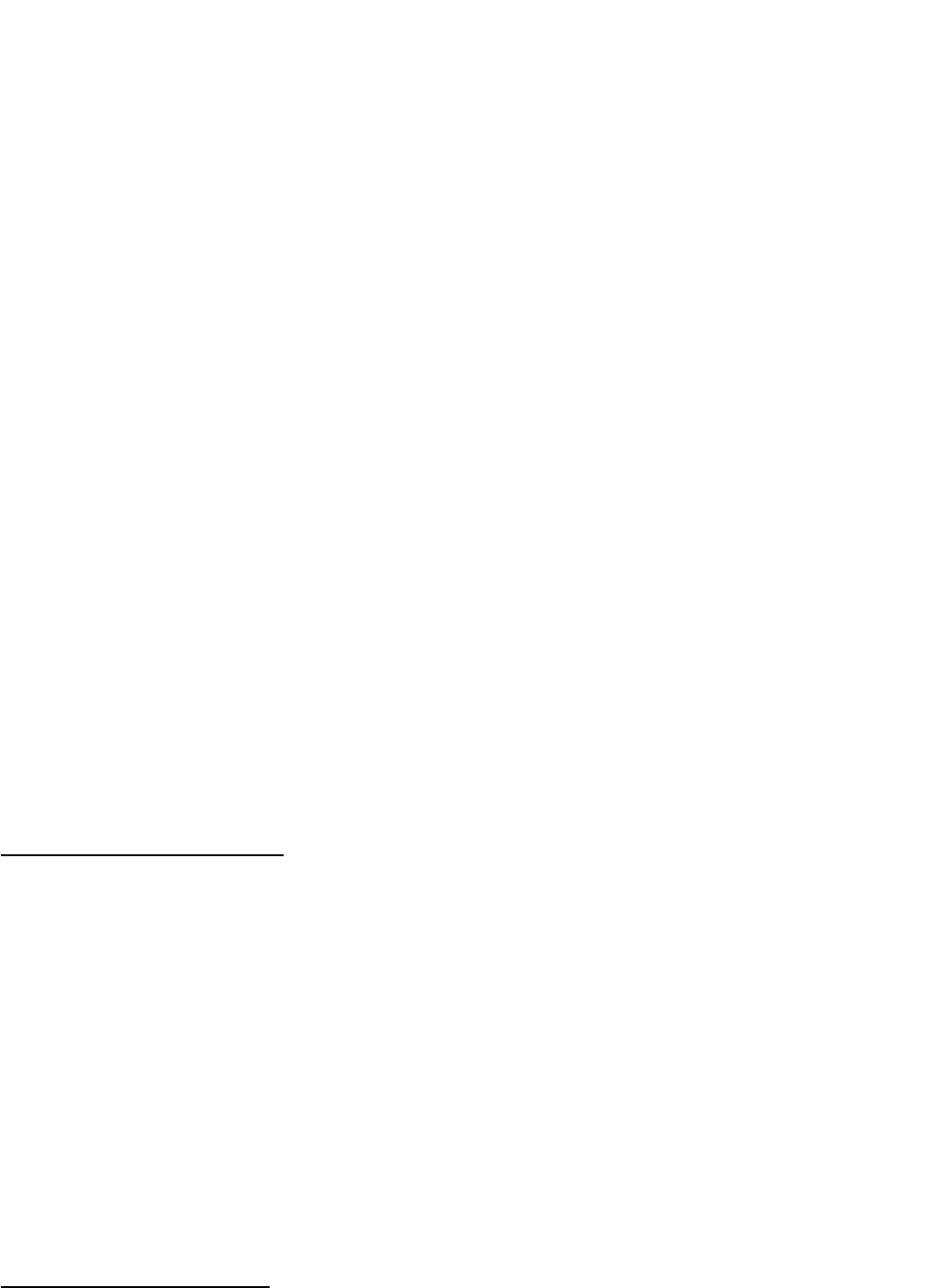
Evaluation and Management Codes Most Likely to be Used by Psychiatrists
Category/Subcategory Code Numbers
Office or outpatient services
New patient 99201–99205
Established patient 99211–99215
Hospital observational services
Observation care discharge services 99217
Initial observation care 99218–99220
Hospital inpatient services
Initial hospital care 99221–99223
Subsequent hospital care 99231–99233
Hospital discharge services 99238–99239
Consultations*
Office consultations 99241–99245
Inpatient consultations 99251–99255
Emergency department services
Emergency department services 99281–99288
Nursing facility services
Initial Nursing Facility Care
Subsequent nursing facility care
Nursing facility discharge services
Annual Nursing Facility Assessment
Domiciliary, rest home, or custodial care services
99304–99306
99307-99310
99315–99316
99318
New patient 99324–99328
Established patient 99334–99337
Home services
New patient 99341–99345
Established patient 99347–99350
-41-
American Psychiatric Association
Office of Healthcare Systems & Financing
800 343 4671 ● [email protected]
Category/Subcategory
Code Numbers
Team conference services
Team conferences with patient/family
Team conferences without patient/family
99366
99367**
Behavior Change Interventions
Smoking and tobacco use cessation
Alcohol and/or Substance abuse structured screening and brief
intervention
99406-99407
99408-99409
Non-Face-to-Face Physician Services**
Telephone services
On-Line Medical Evaluation
Basic Life and/or Disability Evaluation Services
Work Related or Medical Disability Evaluation Services
*Medicare does not pay for the consultation codes
**Medicare covers only face-to-face services
99441-99443
99444
99450
99455-99456
Category/Subcategory
Code Numbers
Team conference services
Team conferences with patient/family
Team conferences without patient/family
99366*
99367
Behavior Change Interventions
Smoking and tobacco use cessation
Alcohol and/or Substance abuse structured screening and brief
intervention
99406-99407
99408-99409
Non-Face-to-Face Physician Services*
Telephone services
On-Line Medical Evaluation
Basic Life and/or Disability Evaluation Services
Work Related or Medical Disability Evaluation Services
*Medicare covers only face-to-face services
99441-99443
99444
99450
99455-99456
